So, let's suppose that the doctor just diagnosed a loved one in my family with this thing called a sacral decubitus ulcer. I just looked it up on-line, and I now know that it’s a bed sore on a person’s backside. It’s caused by constant pressure on a bony area. Healthy, mobile people don't usually get these ulcers because they can wiggle, move around, and alleviate the pressure when their body parts feel numb. I felt similar numbness as a child sitting on wooden church pews and paid the price when I moved too much during a sermon. Oh, life’s invaluable experiences …
I understand the pressure on a bony area, but what about this shear thing? How am I supposed to help heal this ulcer when I can’t understand what causes it?
This is what I found on wiki (www.en.wikipedia.org/wiki/Shear_stress):
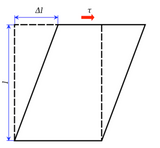
A shear stress, is applied to the top of the square while the bottom is held in place. This stress results in a strain, or deformation, changing the square into a parallelogram. The area involved would be the top of the parallelogram.
The formula to calculate average shear stress is:

where:
 = the shear stress;
= the shear stress;
 = the force applied;
= the force applied;
 = the cross-sectional area of material with area parallel to the applied force vector.
= the cross-sectional area of material with area parallel to the applied force vector.
OK… that really helped me… NOT!
What next? I went to a legitimate pressure ulcer site, the National Pressure Ulcer Advisory Panel, to learn about shear. This is how they define “shear” (www.npuap.org/wp-content/uploads/2012/02/Shear_slides.pdf):
An action or stress resulting from applied forces which causes or tends to cause two contiguous internal parts of the body to deform in the transverse plane (i.e. shear strain)
I guess I understand slightly better now… Right? I read on.
Although shear is understood to be a major contributor to the formation of pressure ulcers, the measurement of shear and how shear contributes to the formation of pressure ulcers have not yet been fully established.
don’t know... how shear actually causes tissue damage.
Huh? They DON’T know how this thing even causes damage… What the…? Where do I go from here? Just a bit more before I throw in the towel …
Shear force occur[s] when the head of the bed is raised and lowered
Reduce the chance of sliding down in the bed
... changes in position or posture are likely to change shear externally and internally
OK, now we’re getting somewhere!
This shear thing come up when the patient moves or is moved, and if I go back to that square thing on wiki, it comes up when there is a force that wants to move the patient but the patient does not move or parts of his body move at different speeds because some part(s) of the patient’s body is/are stuck to the bed… The simplest way I can understand this issue is to imagine a large cube of Jell-O on a plate, and when the top part of that Jello-O cube moves at different speeds or directions than the bottom part that is stuck to the plate, there is shear.
Now that I am seeing the hazy outlines of the dim light at the end of the tunnel, what can I do to minimize shear for a patient? Most patients need to be moved to different mattress incline angles to feed them or let them watch TV, but if that change in inclination causes shear, what solutions are available, besides not changing the inclination? Just having the patients on an incline subjects them to shear stresses because the body wants to slide down into the lowest part of the mattress, but skin friction against the sheets prevents the downward slide in many cases. Frequently, the shear stress is also felt by non-skin tissue, like the tissue attached to the bones that isn't touching the sheets but feels the stress as the rest of the body tries to slump down into the lowest part of the mattress.
One solution is to place the patient on a really slick surface so that the skin and tissue attached to bone are allowed to move at same speeds, like a cube of Jell-O falling in space and no one part of it feels any shear stress against another part. However, such a solution, with our sheets and current healthcare protocols, is impossible or impractical. Another solution is to provide tangential support that is perpendicular to the tissues subject to gravity or movement. For instance, if the plate with the Jell-O cube is moving to the right, a support system, like a saltine cracker covering the whole left side of the Jell-O, will minimize the shear on the Jell-O cube and move the top and bottom of the cube to the right at the same speed as the plate. One way to provide such a tangential support that is perpendicular to the tissue is to use a fluid support system. Fluid systems, with properly designed containment systems, can conform to the changing body forms and dynamically provide near perpendicular support to all contact points along the body surface. Fluids can provide such consistent support because they are incompressible, unlike the compressible mattress materials largely in use today. Since we cannot get rid of mattress sheets to reduce shear and allow our patients to slide frictionless into the mattress fold, products based upon fluid technologies can provide an inexpensive and effective way to minimize shear on patients with or subject to pressure ulcers.